The Bile Duct Injury (BDI) rate with laparoscopic cholecystectomy is reported to be 0.5%1, and while relatively low, when injuries occur, they can be catastrophic.2

The global minimally invasive surgical systems market is expected to grow at a CAGR of 10.9% from 2020 to 2025, driven by the rapidly increasing demand from the patients undergoing minimally invasive surgical procedures, increasing surgical need, and the surge in the prevalence of colorectal and other gastrointestinal diseases.1
New technological advancements, such as miniaturisation of surgical equipment and development of surgical robots, have substantially increased the number of minimally invasive surgeries performed across the world.

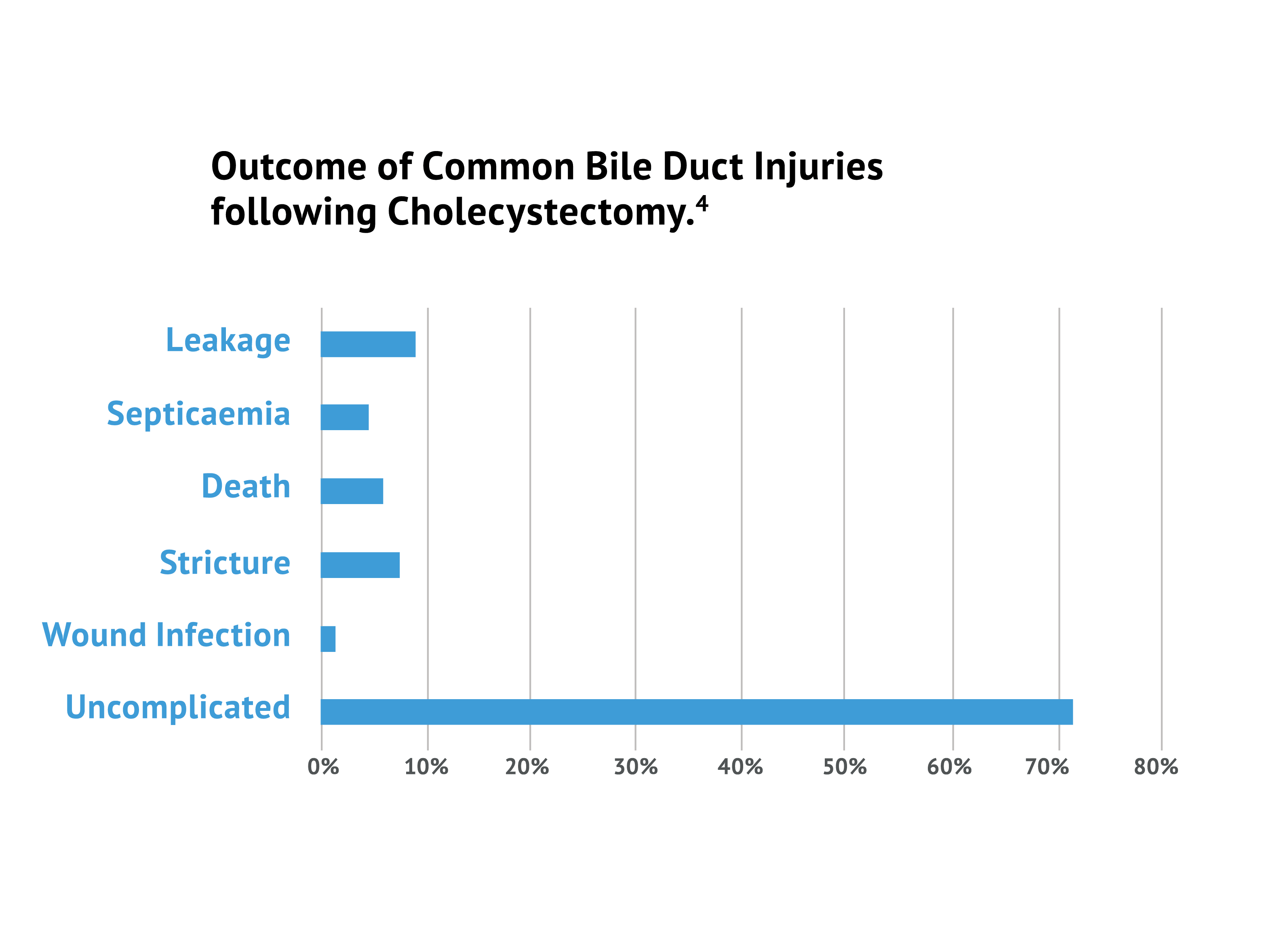
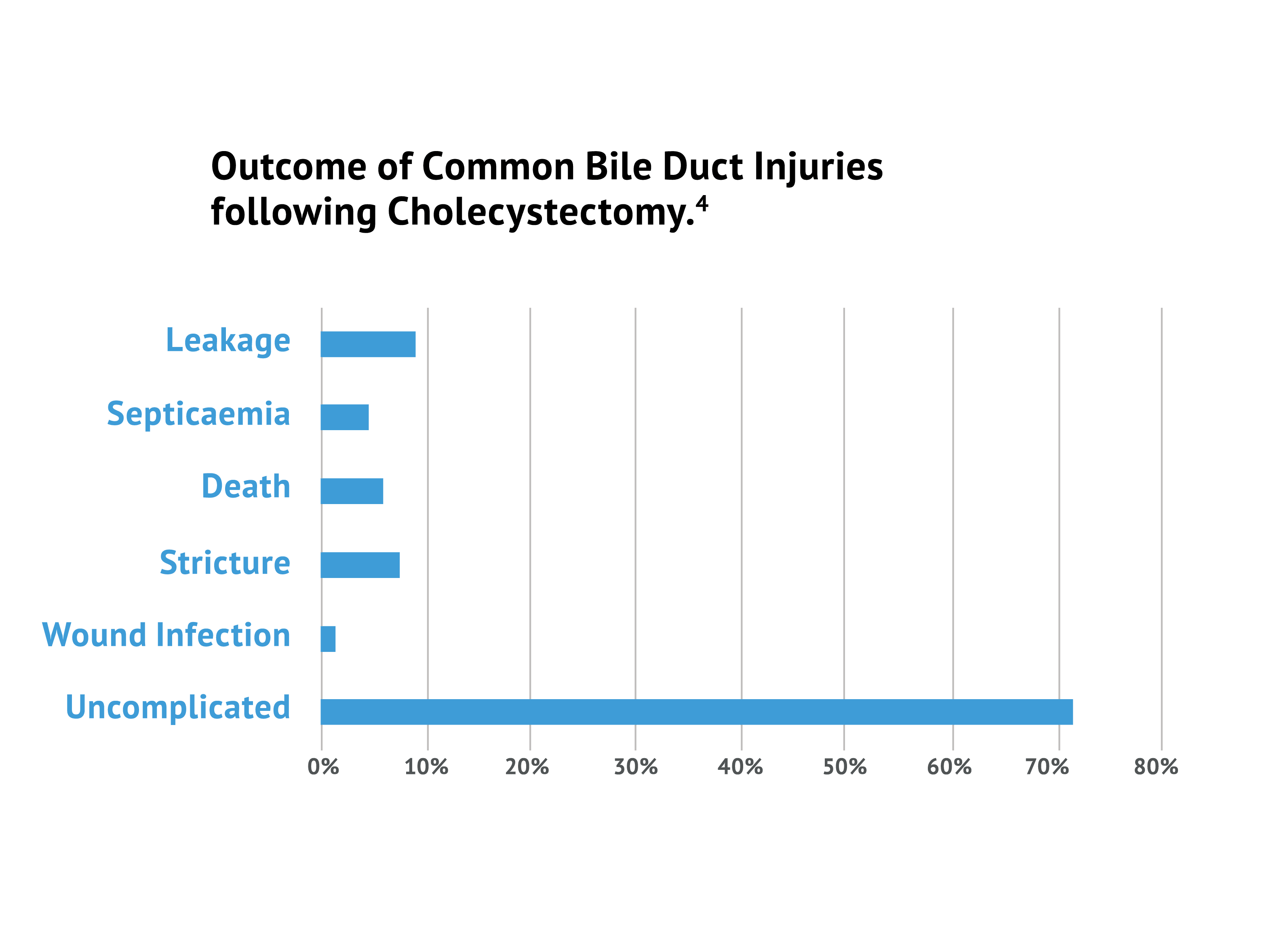
The Bile Duct Injury (BDI) rate with laparoscopic cholecystectomy is reported to be 0.5%1, and while relatively low, when injuries occur, they can be catastrophic.2
The primary cause of error in 97% of cases was a visual perception illusion.3
Surgeons had a 3-fold improvement in ability to visualise critical bile duct structures using ICG.4
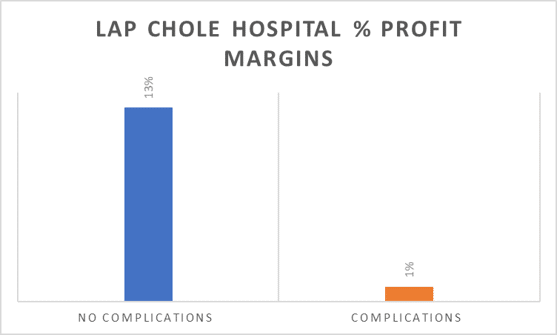
Profit margins at hospitals drop from 13% to 1% when complications in lap chole surgeries occur.5

X-Ray Cholangiography has been used in the past to overcome this visualisation problem. However it has drawbacks that are not apparent with Indocyanine Green (ICG) use.
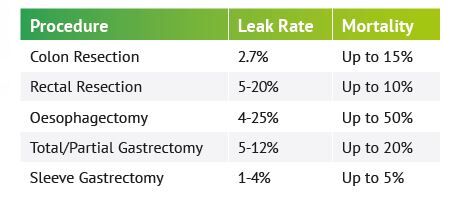
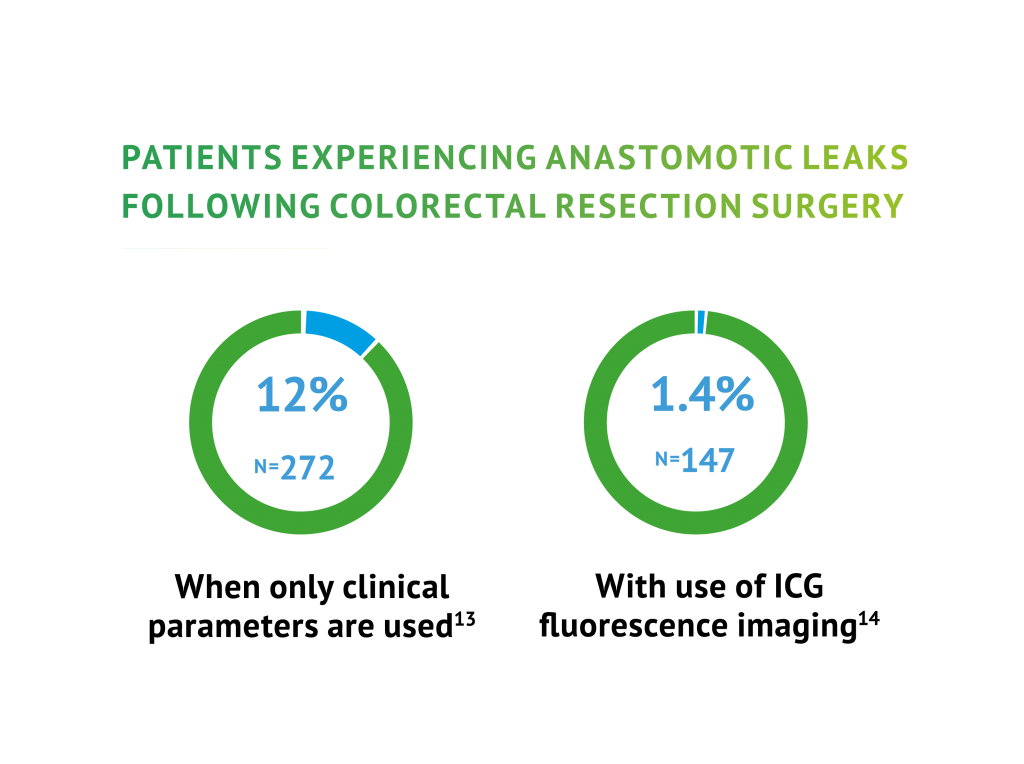
Colorectal surgery frequently involves bowel resection with restoration of the alimentary tract by anastomosis. Indocyanine green (ICG) fluorescence imaging has proven to be an effective tool to assess anastomotic perfusion. Its use for the prevention of anastomotic leaks (AL) has been gaining popularity, with accumulating data on lower leak rates with (ICG) fluorescence guided surgery.9
Most common methods used to evaluate the perfusion status of the colon has been to visually observe the change in colour of the colon wall with the surgeon’s naked eye and to carefully observe the pulse of the colon wall. However, these methods are subjective and not always accurate.
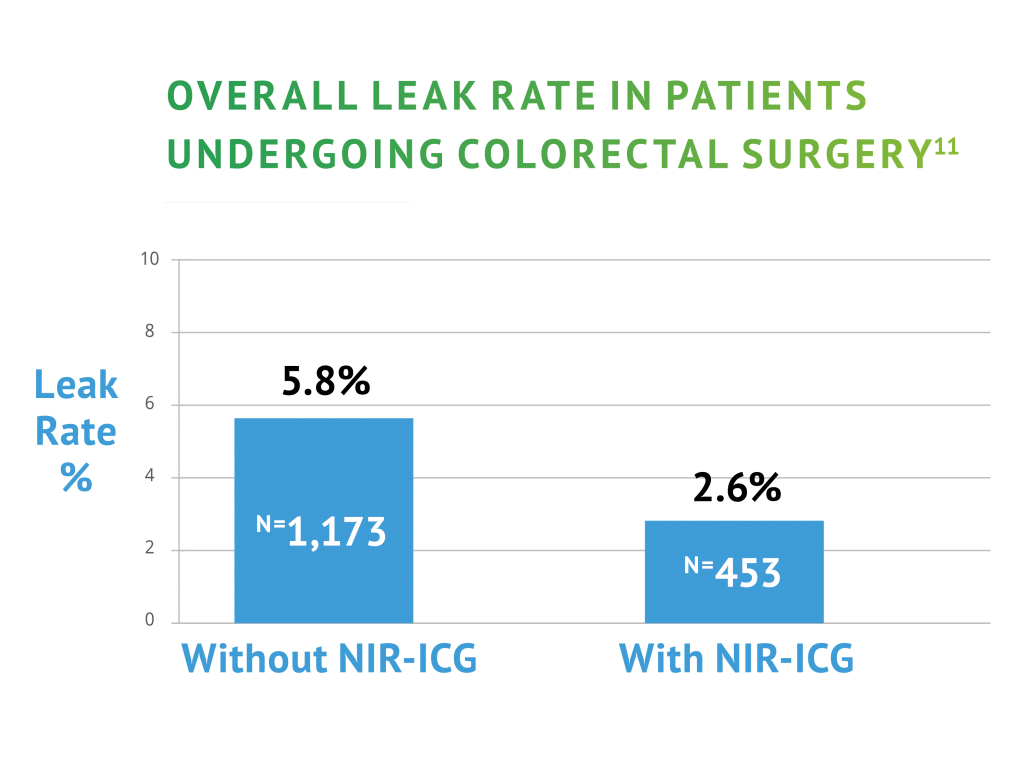
Reported rates of anastomotic leakage vary from 3-6% in experienced colorectal surgeons and 3-25% overall.10 Combining the use of ICG with a near-infra red (NIR) laparocsopic camera system offers the surgeon the possibility of an objective, real-time assessment of blood flow to the colon.
ICG Proven to reduce leak rates in Colorectal Surgery
There is a growing body of evidence that proves the significant value of using ICG in colorectal surgery.
Below is a summary of two recent Clinical Trials proving that ICG is safe, effective and is increasingly viewed as the gold standard in laparoscopic colorectal procedures.
Name of the Medicinal Product
Verdye 5 mg/ml Injection 25 mg / 50 mg, Powder for Solution
Pharmaceutical Form
Powder for Solution for Injection Dark-green powder
Therapeutic indications
This medicinal product is for diagnostic use only.
Method of administration
Before administration the powder must be reconstituted with water for injection.
Shelf Life
5 years. After reconstitution, the solution should be used immediately, protected from light.
Diagnostic Indications
Cardiac, circulatory and micro-circulatory diagnostics
Liver function diagnostics
Ophthalmic angiography diagnostics
All references available in the MIS brochure download