Background: The safety and efficiency of minimally invasive approaches for liver resection have been confirmed (Wakabayashi in Ann Surg, 2015). However, laparoscopy suffers from several limitations due to technical difficulties, particularly for difficult hepatectomy with lymphadenectomy, biliary, and vascular reconstruction. Robotic assets could improve accessibility for difficult liver resections. Patients and methods: A 56-year-old woman was treated for a hilar cholangiocarcinoma, Bismuth 3b.
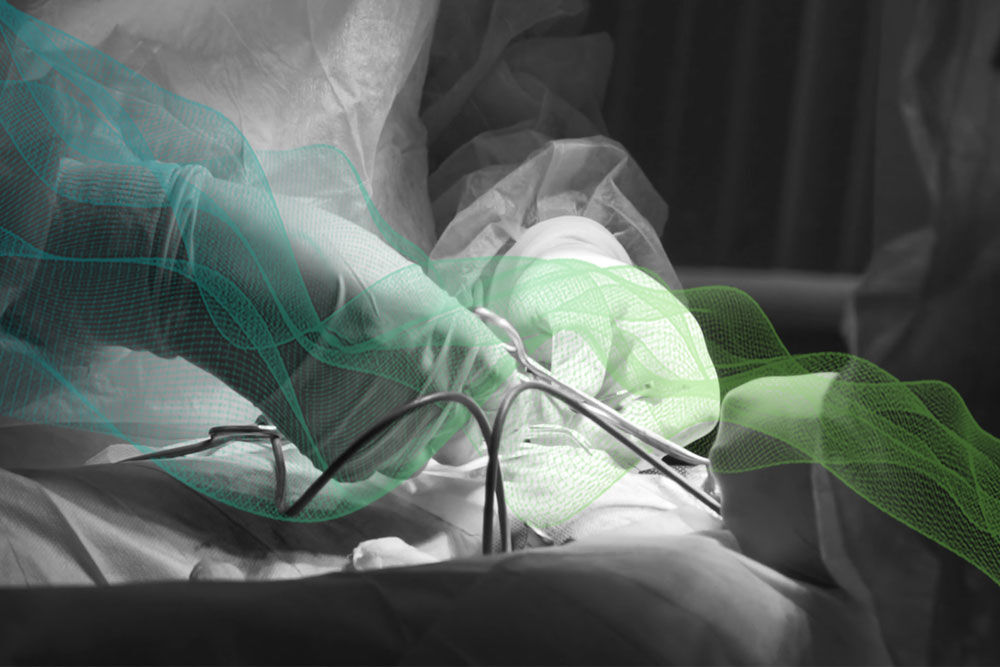
Results: A robotic anatomical left hepatectomy extended to caudate lobe and common biliary duct was decided. A Da Vinci X robot was used. The procedure was performed with a second surgeon positioned between the patient’s legs. Left hepatectomy was extended to common biliary duct and caudate lobe. A four-hands parenchymal dissection (Camerlo in J Robot Surg, 2020) was performed with laparoscopic ultrasonic dissector and robotic irrigated bipolar, guided by indocyanine green. Axis of deep transection line was maintained using the EndoWrist function and exposure with a fourth arm. No pedicle clamping was necessary. Segment 1 was released with a mediocaudal approach. Lateral portal vein resection was performed after parenchymal transection was completed. Hepaticojejunostomy was done separately to the right anterior and posterior biliary duct. Operation time was 420 min, and estimated blood loss was 100 ml. The postoperative course was uneventful. The patient was discharged on postoperative day 8. Pathological findings revealed a 15-mm hilar cholangiocarcinoma with complete resection and eight lymph nodes, all negative.
Conclusions: Robotic approaches could improve accessibility to minimally invasive liver resection of Klatskin tumor.