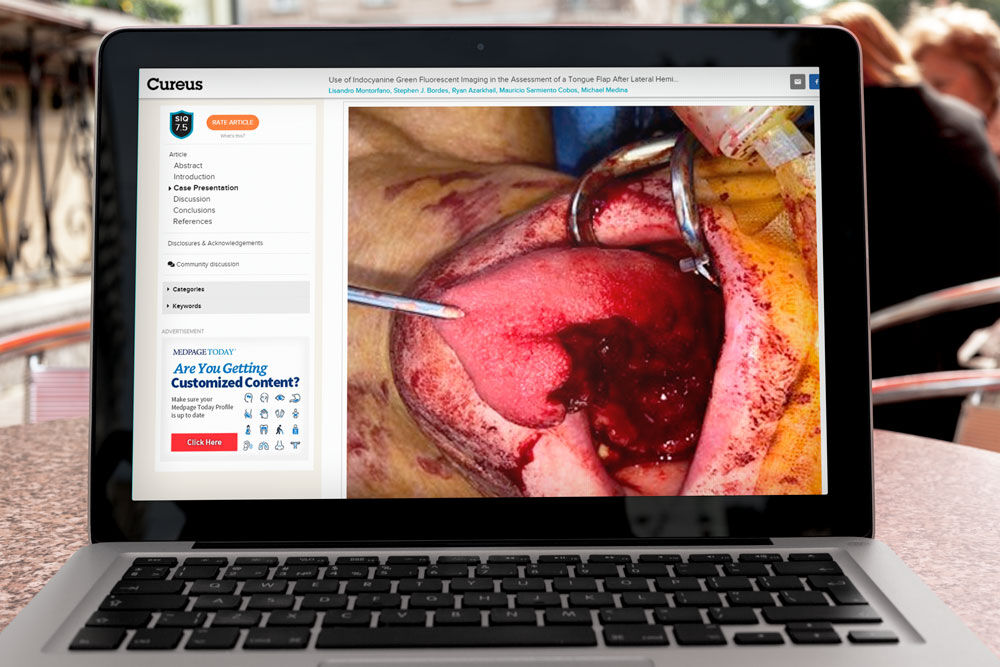
Recent paper published in British Journal of Surgery which undertook an assessment of anastomotic blood perfusion with intraoperative indocyanine green fluorescence angiography (ICG-FA) to evaluate if it may be effective in preventing anastomotic leak compared with standard intraoperative methods in colorectal surgery.
MEDLINE, PubMed, Cochrane Central Register of Controlled Trials and the Cochrane Library were searched for RCTs and observational studies on intraoperative ICG-FA to May 2020.
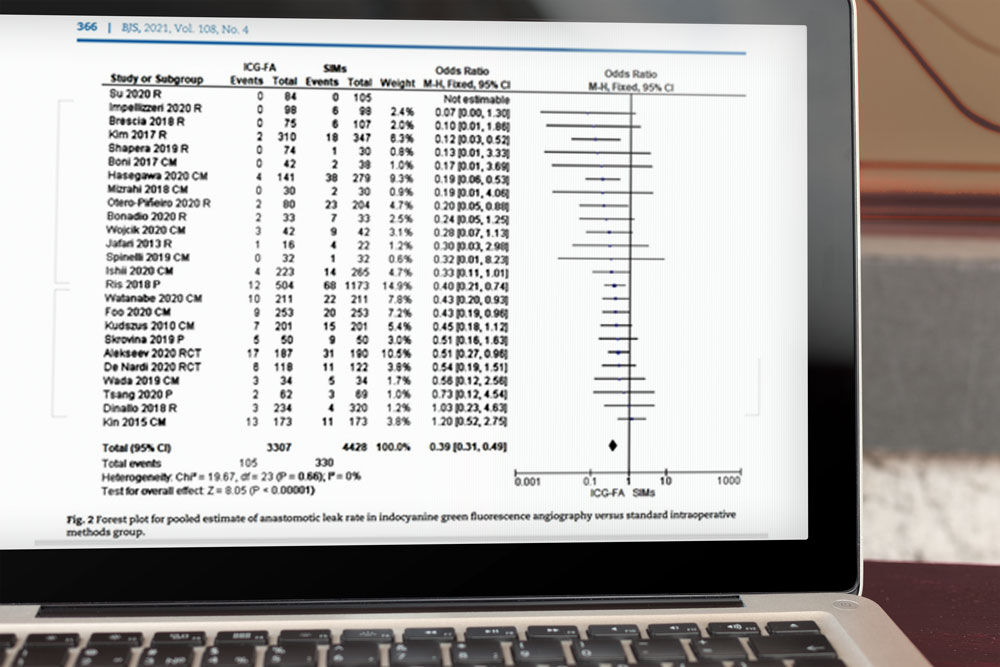
Results: Twenty-five comparative studies included a total of 7735 patients. The use of intraoperative ICG fluorescence angiography was linked with a significant reduction in all grades anastomotic leak (OR 0.39 (95 per cent c.i. 0.31 to 0.49), P < 0.001; number needed to treat for an additional beneficial outcome (NNTB) 23) and length of hospital stay (MD -0.72 (95 per cent c.i. -1.22 to -0.21) days, P = 0.006). A significantly lower incidence of grade A (OR 0.33 (0.18 to 0.60), P < 0.001), grade B (OR 0.58 (0.35 to 0.97), P = 0.04) and grade C (OR 0.59 (0.38 to 0.92), P = 0.02) anastomotic leak was demonstrated in favour of ICG-FA. For low or ultra-low rectal resection, the odds of developing anastomotic leakage was 0.32 (0.23 to 0.45) (P < 0.001; NNTB 14). There were no differences in duration of surgery, and no adverse events related to ICG fluorescent injection.
Conclusion: The use of ICG-FA instead of standard intraoperative methods to assess anastomosis blood perfusion in colorectal surgery leads to a significant reduction in anastomotic leakage and in the need for surgical reintervention for anastomotic leak, especially in patients with low or ultra-low rectal resections.