Background: Near-infrared fluorescent cholangiography (NIRFC) with indocyanine green (ICG) as the developer yields clear visualization of the extrahepatic bile ducts and is effective in identifying key structures. Here, we analyzed and compared the surgical outcomes of fluorescent and conventional laparoscopy in cholecystectomy of various difficulties and then assessed the value of NIRFC.
Results: This study included a total of 624 patients. The patients were classified into the ICG group (n = 218) and the non-ICG group (n = 218) after a 1:1 ratio PSM. Our data showed significant differences between the groups in operative time (P = 0.020), blood loss (P = 0.016), length of stay (P = 0.036), and adverse reaction (P = 0.023). Stratified analysis demonstrated that ICG did not significantly improve the surgical outcomes in simple cases (n = 208). On the other hand, in difficult cases (n = 228), NIRFC shortened operative time (P = 0.003) and length of stay (P = 0.015), reduced blood loss (P = 0.028) and drain placement rate (P = 0.015), and had fewer adverse reactions (P = 0.023). The data showed that five cases were converted to laparotomy while two cases had minor bile leaks in the non-ICG group. There was no bile duct injury (BDI) in all the cases. Furthermore, high BMI, history of urgent admission and abdominal surgery, palpable gallbladder, thickened wall, and pericholecystic collection were risk factors for surgical difficulty.
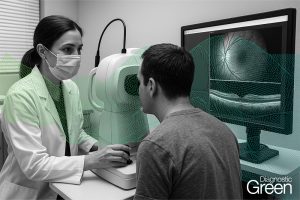
Conclusion: ICG-assisted NIRFC provides real-time biliary visualization. In complicated conditions such as acute severe inflammation, dense adhesions, and biliary variants, the navigating ability of fluorescence can enhance the operation progress, reduce the possibility of conversion or serious complications, and improve the efficiency and safety of difficult LC.